StrongMinds
StrongMinds
Introduction
StrongMinds focuses on women and adolescents in sub‑Saharan Africa who suffer from depression but have little or no access to mental‑health care. The organization delivers group interpersonal psychotherapy (IPT‑G): structured, time‑limited group counselling that helps participants understand the roots of their depression, improve relationships, and build practical coping skills. External analyses using well‑being‑adjusted life years (WELLBYs) suggest that StrongMinds’ program creates large gains in life satisfaction at a lower cost per person than most traditional mental‑health services, and several times the impact of simply giving people cash, though still below the very top global health charities.
The problem: widespread, untreated depression
Depression is one of the leading causes of disability worldwide, and in countries like Uganda and Zambia it is extremely common among women living in poverty. Yet public health systems in these settings devote very limited resources to mental health, leaving an estimated 80–90% of people with depression without any effective treatment at all. Untreated depression does not just cause intense emotional suffering; it also harms physical health, parenting, employment, and social relationships, meaning that one person’s illness can drag down the well‑being and economic prospects of an entire household.
In low‑income communities, women with depression often face stigma and misunderstanding, which can further isolate them and make it less likely they will seek or receive help. Where services do exist, they are frequently centralized in urban hospitals, delivered by scarce specialists, and priced out of reach for poorer households. This combination of high need, low access, and severe downstream consequences means that affordable, scalable mental‑health treatments could have outsized benefits if they can be delivered effectively in these contexts.
The solution: low‑cost, scalable psychotherapy
StrongMinds’ solution is to provide a proven form of talk therapy (group interpersonal psychotherapy) in a way that is adapted for low‑resource settings and can be scaled to reach hundreds of thousands of people. Instead of relying on psychiatrists or clinical psychologists, StrongMinds trains lay community workers and partner staff to deliver therapy in groups, dramatically reducing costs while still following a structured, evidence‑based protocol. Group formats allow many more women to be treated per facilitator and also create social support networks among participants, which can persist beyond the formal therapy sessions.
Independent analysts who evaluate charities on cost‑effectiveness have translated StrongMinds’ mental‑health impacts into WELLBYs, a metric based on changes in self‑reported life satisfaction. Using conservative assumptions about publication bias, social desirability, spillover effects on family members, and reduced effectiveness at scale, one prominent assessment estimates that StrongMinds produces about 17 life‑satisfaction point‑years per US$1,000 donated—more than double the impact of direct cash transfers measured in the same units. This suggests that, for donors who care particularly about mental health and subjective well‑being, funding scalable psychotherapy can be an especially powerful way to improve lives.


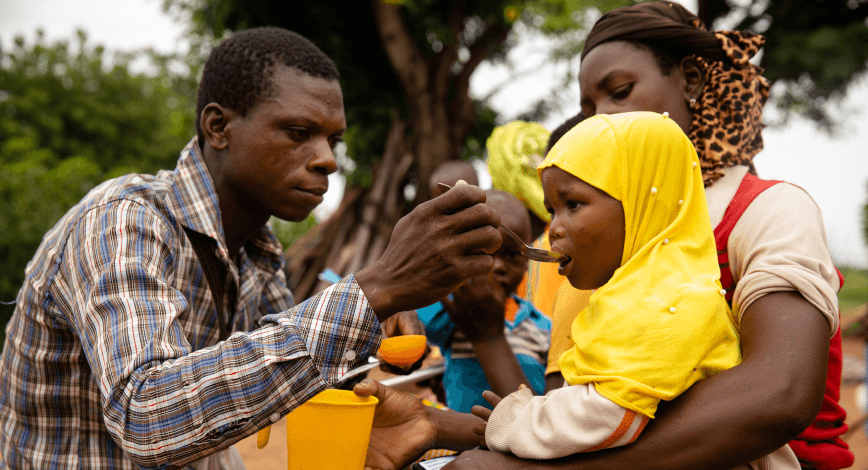
StrongMinds democratizes access to mental health care for people with depression globally.
How StrongMinds works
StrongMinds’ model begins with community‑based identification of women and adolescents showing signs of depression, often through local partners, community events, or screening in schools and health facilities. Those who screen positive are invited to join small therapy groups, typically consisting of five to ten participants who share similar backgrounds and challenges. Groups meet for approximately 90 minutes, once or twice a week, over four to eight weeks, either in person or via phone when in‑person meetings are not feasible.
During sessions, facilitators use the IPT‑G framework to help participants link their mood to key life events and relationship problems, identify specific interpersonal issues (such as conflict, grief, role transitions, or social isolation), and practice new ways of communicating and solving problems. The structured nature of IPT‑G means that lay facilitators can be trained to deliver it consistently, while still allowing space for participants to share their experiences and support one another. Over the course of the program, many participants move from severe or moderate depression to minimal or no symptoms, and follow‑up data suggest that a substantial proportion remain depression‑free months after treatment ends.
StrongMinds also invests in partnerships and systems that amplify its reach. By training staff in other NGOs, collaborating with governments, and integrating its model into schools and health services, the organization can extend therapy to many more people than it could reach through its own direct implementation alone. As it scales, StrongMinds has reported declining costs per person treated (for example, citing a cost around US$105 per patient in 2022 and aiming lower as efficiencies grow), which further improves its cost‑effectiveness and allows donor funds to stretch to more women and adolescents in need.
Introduction
StrongMinds focuses on women and adolescents in sub‑Saharan Africa who suffer from depression but have little or no access to mental‑health care. The organization delivers group interpersonal psychotherapy (IPT‑G): structured, time‑limited group counselling that helps participants understand the roots of their depression, improve relationships, and build practical coping skills. External analyses using well‑being‑adjusted life years (WELLBYs) suggest that StrongMinds’ program creates large gains in life satisfaction at a lower cost per person than most traditional mental‑health services, and several times the impact of simply giving people cash, though still below the very top global health charities.
The problem: widespread, untreated depression
Depression is one of the leading causes of disability worldwide, and in countries like Uganda and Zambia it is extremely common among women living in poverty. Yet public health systems in these settings devote very limited resources to mental health, leaving an estimated 80–90% of people with depression without any effective treatment at all. Untreated depression does not just cause intense emotional suffering; it also harms physical health, parenting, employment, and social relationships, meaning that one person’s illness can drag down the well‑being and economic prospects of an entire household.
In low‑income communities, women with depression often face stigma and misunderstanding, which can further isolate them and make it less likely they will seek or receive help. Where services do exist, they are frequently centralized in urban hospitals, delivered by scarce specialists, and priced out of reach for poorer households. This combination of high need, low access, and severe downstream consequences means that affordable, scalable mental‑health treatments could have outsized benefits if they can be delivered effectively in these contexts.
The solution: low‑cost, scalable psychotherapy
StrongMinds’ solution is to provide a proven form of talk therapy (group interpersonal psychotherapy) in a way that is adapted for low‑resource settings and can be scaled to reach hundreds of thousands of people. Instead of relying on psychiatrists or clinical psychologists, StrongMinds trains lay community workers and partner staff to deliver therapy in groups, dramatically reducing costs while still following a structured, evidence‑based protocol. Group formats allow many more women to be treated per facilitator and also create social support networks among participants, which can persist beyond the formal therapy sessions.
Independent analysts who evaluate charities on cost‑effectiveness have translated StrongMinds’ mental‑health impacts into WELLBYs, a metric based on changes in self‑reported life satisfaction. Using conservative assumptions about publication bias, social desirability, spillover effects on family members, and reduced effectiveness at scale, one prominent assessment estimates that StrongMinds produces about 17 life‑satisfaction point‑years per US$1,000 donated—more than double the impact of direct cash transfers measured in the same units. This suggests that, for donors who care particularly about mental health and subjective well‑being, funding scalable psychotherapy can be an especially powerful way to improve lives.

StrongMinds democratizes access to mental health care for people with depression globally.
How StrongMinds works
StrongMinds’ model begins with community‑based identification of women and adolescents showing signs of depression, often through local partners, community events, or screening in schools and health facilities. Those who screen positive are invited to join small therapy groups, typically consisting of five to ten participants who share similar backgrounds and challenges. Groups meet for approximately 90 minutes, once or twice a week, over four to eight weeks, either in person or via phone when in‑person meetings are not feasible.
During sessions, facilitators use the IPT‑G framework to help participants link their mood to key life events and relationship problems, identify specific interpersonal issues (such as conflict, grief, role transitions, or social isolation), and practice new ways of communicating and solving problems. The structured nature of IPT‑G means that lay facilitators can be trained to deliver it consistently, while still allowing space for participants to share their experiences and support one another. Over the course of the program, many participants move from severe or moderate depression to minimal or no symptoms, and follow‑up data suggest that a substantial proportion remain depression‑free months after treatment ends.
StrongMinds also invests in partnerships and systems that amplify its reach. By training staff in other NGOs, collaborating with governments, and integrating its model into schools and health services, the organization can extend therapy to many more people than it could reach through its own direct implementation alone. As it scales, StrongMinds has reported declining costs per person treated (for example, citing a cost around US$105 per patient in 2022 and aiming lower as efficiencies grow), which further improves its cost‑effectiveness and allows donor funds to stretch to more women and adolescents in need.